The Role of EMPI Services in Data Conversion for Health Information
When it comes to data conversion for health information (PHI), there are many aspects to consider to ensure …
The process of legacy EHR system retirement can bring a host of challenges. Multiple questions arise as a result, and hospital administrators have to answer important questions on how to handle different data records or which data should be specifically moved to the new EHR system, and so on. A health organization must make sure that they are following state-specific requirements (if any) as well as all the federal guidelines related to data retention. The entire data transfer process, which includes data extraction, conversion, and retention, involves creating proper strategies for each of these procedures to successfully transfer historical records to the new legacy system.
Through this article, you will be able to explore:
The process of transitioning from one EHR/EMR is often filled with challenges. When the legacy applications are required to be retired, there are critical decisions that have to be made. Data management is one of the essential considerations in this aspect. While some managers of health information prefer the practice of archiving old legacy data and applications, others might just try to move data en masse into a new EHR. There are certain merits attached to each of the approaches. But, the best approach is the practice of data archiving and migration in a balanced combination.
The practice of data extraction has huge potential for healthcare applications in terms of allowing health policies to utilize data regularly and recognizing disorganizations. These are the best methods for enhancing care and decreasing expenses. Some of the most advanced and best strategies for data extraction are:
1. Using NLP for text notes: Natural language processing or NLP is a strategy for extracting data from clinical notes in a format that is free-text form. Generally, algorithms of machine learning work best on data that are structured. However, tons of relevant information could be obtained from documents that are text free and written in an unstructured way. Through algorithms of NLP, relevant keywords that are healthcare-specific could be found in a document of text. These include the likes of clinical and diagnosis procedures, drug codes, and so on. The algorithm could help in resolving the data into a single record after obtaining them from clinical notes. The patterns could be then made evident using applications of machine learning.
2. Investing in APIs: The process of health data extraction could be simplified with the help of an API or Application Programming Interface. One can extract data from an EMR with the help of APIs and then transfer it for archiving purposes or send it to another application. Similarly, patients would be able to compile and access their data from various providers and then view them through a single portal. The compiled data would allow the physicians to make effective recommendations and decisions from complete information. APIs can help physicians in extracting relevant portions of information rather than exchanging information about a patient having hundreds of documented pages. These relevant portions could be selected by the physicians for the specialists when they need to exchange patient information to connect the latter’s EHR to the physician’s EHR and pick the pertinent information for the treatment of the patient.
3. Using AI for extracting data: Various tools of AI or Artificial Intelligence are being developed for extracting value from the real-world evidence that is embedded in unstructured data of EHR. According to a study, scientists from the University of Michigan came up with a framework for preprocessing extracted data from EHR. The essence of the framework involves- Missing values, multiple types of data, sampled data irregularities, and unstructured data. Making use of a preprocessor for EHR data extraction could help in preparing the data into a format that is suitable for establishing machine learning techniques.
Project planning: Successful projects of migration requires planning. There are grave consequences to migrating data incorrectly. Data could become inaccessible for providers, which could directly hamper the quality of healthcare services given to patients. Without proper project planning, there might be errors in the migrated data, which, when discovered during quality assurance, can turn into a nightmare. It might take up months to fix it because of the involved work, workflow disruption, and the costs involved in moving data.
Downtime planning: Just as project planning is necessary, it is also important to plan the scheduled time when the migration infrastructure or equipment is shut down or limited in order to undergo planned repairs, upgrades, maintenance, or testing. Downtime planning would help in minimizing the confusion and frustration regarding why a technology is unavailable at a certain point of time. Through planned maintenance, the overall amount of downtime is reduced, and the technologies are kept in a healthy condition.
Data validation: Data validation refers to checking the quality and accuracy of source data before using it for migration. Data validation forms an essential part of any data handling process, and it is no exception here. If there is no accuracy in the data from the start, there would be inaccuracy in the migrated data as well. Validating the clarity, accuracy, and details of the data would not only help in mitigating any project defects but also would not negatively impact decisions that are taken based on the migrated data.
Some of the best practices to follow for secure archiving of data are:
Having a backup: It is extremely important to have a secure backup during the archival procedure. There are always possibilities of archives being vulnerable to ransomware hacking. Backing up the data would keep all the data safe.
Sorting and identifying the data before archiving: Before the healthcare data is archived, one should check out the data and create an inventory accordingly. Categorizing the data, prioritizing it, and then considering carefully which data would be needed for a certain ongoing operation and which ones to be moved would make the archiving process even more efficient.
Ensuring the archival process is compliant with regulations of record retention: Being compliant with the record retention regulations does not just mean the records are there somewhere. There needs to be a storage system that would protect all the PHI or Protected Health Information.
Selecting an option for handling all types of files: Archives of healthcare data are not just restricted to documents. It might also include a lot of other formats like images and so on. While transferring the records to an archive, it would not be suitable if it could accept only a limited file type number.
Seeking out a system with permissions that are user-level: There could be a variant number of users and multiple locations present. However, it may not be required to give all of them the same permissions. Thus it must be ensured that the archiving solution is done in such a way that it allows managing accessibility, i.e., who has access to what document and what kind of access.
Managing legacy data is important for facilitating data transition to new systems of EHR. Effective management of legacy data is critical for minimizing disruptions during EHR replacement and ensuring that patient safety is not jeopardized due to the transition. In order to effectively manage legacy data, one of the first steps would be to develop a plan for converting EHR data to a new system in an automated way. Apart from focusing on electronic data conversion, some of the other strategies to follow for efficient legacy data management include archiving the legacy data and manual data abstraction. The process for developing the conversion plan to a new EHR system should begin before the new EHR system is launched to ensure continuity of care.
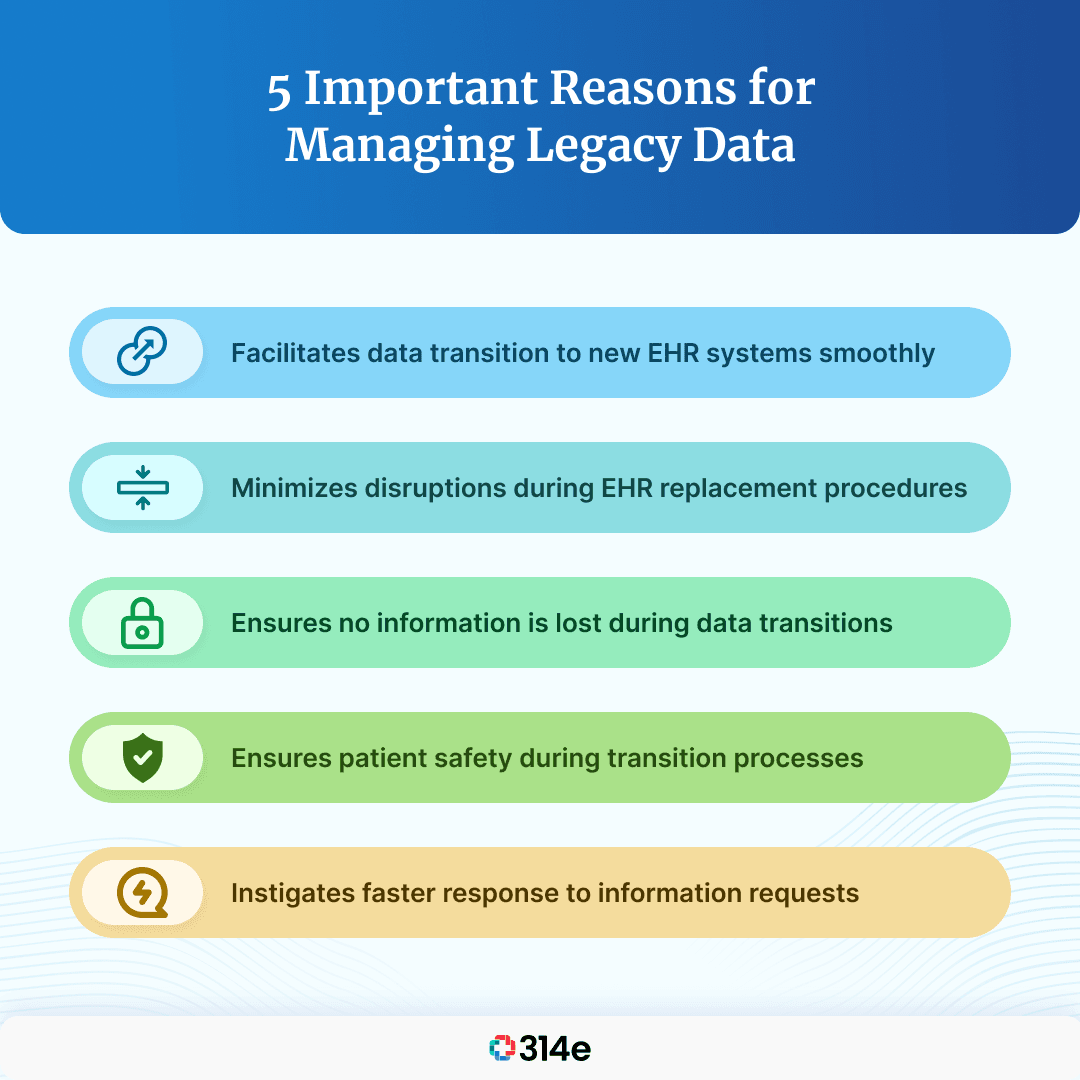
Health officials must decide which elements of data should be transferred automatically to the replacement system and which should not. However, it is important to note that all EHR data cannot be converted automatically. To facilitate the process of data conversion electronically, officials of healthcare must communicate with stakeholders right from the replacement process conception to manage the expectations regarding the legacy data transitioning. Validation of converted data and testing should also be performed by organizations to reach out to the legacy vendors for support purposes. Healthcare organizations work on establishing a manual process of data abstraction for maintaining patient safety and continuity of care.
Join over 3,200 subscribers and keep up-to-date with the latest innovations & best practices in Healthcare IT.
When it comes to data conversion for health information (PHI), there are many aspects to consider to ensure …
Digitization has revolutionized our every day, and while it is true that it has improved efficiency, it is …

The relationship that your health system shares with the archive vendors is as crucial a process as health …