Choosing Your Ideal Healthcare Data Archival Solution
Since the release of the Cures Act Final Rule in May 2020, the US healthcare industry has been experiencing a …

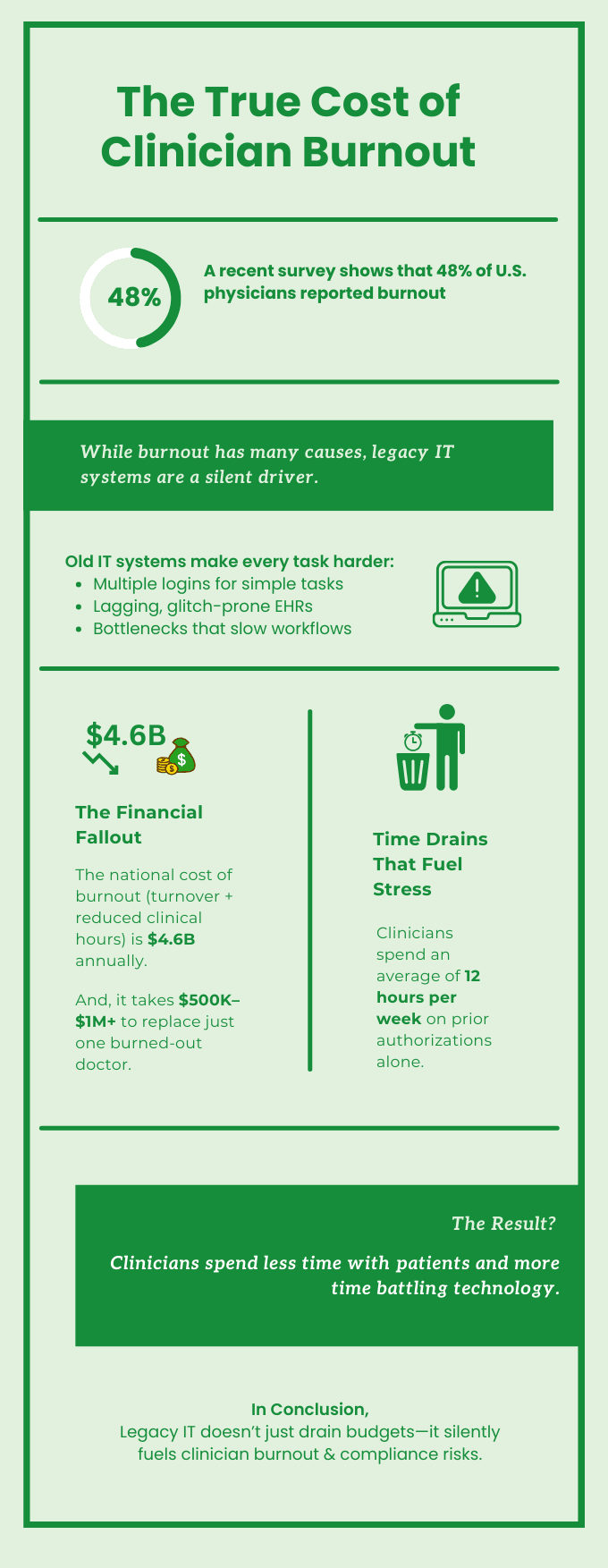
Burnout and compliance failures remain two of the most pressing—and costly—challenges in U.S. healthcare today. While clinician burnout has been widely acknowledged as a crisis, one of its hidden accelerators often goes unaddressed: legacy healthcare systems. Legacy technology, once the backbone of healthcare operations, has now become a source of daily frustration, financial strain, and heightened compliance risks in healthcare.
Instead of streamlining care, these outdated systems slow down workflows, complicate compliance, and drain budgets that could otherwise fund innovation. The result? Clinicians struggling with inefficient tools, organizations exposed to regulatory and financial penalties, and patients caught in the middle.
The numbers speak for themselves:
This blog explores how legacy systems in healthcare silently drive both burnout and compliance risks—and why modern, FHIR-native healthcare data archival solutions are key to breaking this cycle.
In This Blog, We’ll Explore:
entrenched in daily operations. More than 70% of large healthcare systems still rely on outdated platforms, and 60% of U.S. hospitals continue to run at least one critical application on legacy software.
Many large organizations operate with as many as 1,000 unique applications, a significant portion of which are outdated, siloed, and costly to maintain.
The financial and operational strain of maintaining legacy systems is immense. Legacy upkeep swallows up to 75% of IT budgets, with the average cost per system reaching $30 million annually. On a global scale, outdated technology drains an estimated $1.14 trillion every year. And it doesn’t end there—around 40% of IT spending is tied up in technical debt, money that could instead power modernizing legacy systems, interoperability, and better patient care.
1.1. Healthcare’s Heavy Dependence on Legacy Systems:

But the cost isn’t just financial. For clinicians, legacy systems translate directly into daily frustration. Sluggish EHRs, endless logins, and fragmented data silos turn straightforward tasks into time-consuming hurdles. What should be seamless patient workflows become repetitive documentation, manual reconciliations, and clunky workarounds—stealing precious time that could be spent with patients.
And inefficiency is only the beginning. Outdated systems are harder to secure and integrate. Nearly 36% of organizations report higher security vulnerabilities, greater data integration challenges, and a growing risk of outages or system failures. Each slowdown, downtime, or cyber incident doesn’t just affect compliance—it heightens stress for clinicians who are left battling screens instead of caring for patients.
In short, legacy IT systems do more than drain budgets. They quietly magnify regulatory compliance risks, fuel burnout, and erode the very foundation of patient-first healthcare. Decommissioning legacy systems isn’t just a technical upgrade—it’s a critical step toward financial sustainability, workforce resilience, and safer patient care.
If legacy systems in healthcare drain budgets and frustrate clinicians, they also create a minefield for compliance. Outdated platforms simply can’t keep pace with evolving regulations like HIPAA, HITECH, and OCR requirements. Every aging application becomes a liability—an open door to costly fines, penalties, and reputational damage that no healthcare organization can afford.
But the compliance struggle doesn’t stop with regulations. Legacy systems also trap information in silos, making data retrieval during audits painfully slow. What should be a straightforward process turns into a scavenger hunt—delaying responses, raising red flags, and increasing operational risk.
For already stretched clinical and compliance teams, this lack of transparency adds yet another layer of stress. Instead of focusing on care or strategic oversight, staff are buried under extra documentation, manual lookups, and administrative headaches. The result? Reduced efficiency, mounting frustration, and a workforce pushed closer to clinician burnout.
To truly break the cycle of burnout and compliance risk, healthcare organizations must go beyond patchwork fixes and retire legacy systems strategically. Holding on to outdated applications only prolongs inefficiencies, compliance risks, and IT overspending. The key is to preserve what matters most—historical patient data—while eliminating the burden of maintaining obsolete systems.
This is where a FHIR-native healthcare data archival solution delivers transformative value. By leveraging the FHIR standard, archival platforms allow organizations to safely decommission legacy systems without losing critical information. Unlike static or proprietary storage methods, they keep archived data usable, auditable, and accessible across systems for both clinicians and compliance teams.

A modern FHIR-native archival solution provides a secure, cost-effective path forward by enabling organizations to:
FHIR-native, cloud-based healthcare data archival solutions like Muspell Archive are built specifically to help health organizations overcome the setbacks of legacy systems. Designed with compliance, clinician experience, and future interoperability in mind, Muspell Archive empowers healthcare systems to:
With Muspell Archive, organizations gain the ability to sunset legacy applications without compromising compliance or clinician workflows. The result is a foundation for sustainable, patient-first healthcare—where clinicians can focus on care, not clunky systems. Healthcare leaders exploring legacy system retirement and improving clinician workflows, can see Muspell Archive in action through a quick demo.
Legacy healthcare systems may have once powered hospitals and clinics, but today they are among the biggest obstacles to clinician satisfaction, compliance success, and operational efficiency. They sap budgets, slow down workflows, expose vulnerabilities, and force clinicians into time-wasting, frustrating tasks that fuel burnout.
The path forward lies in decommissioning legacy systems and adopting modern, FHIR-native healthcare data archival solutions. By doing so, healthcare organizations not only strengthen compliance in healthcare and reduce risk but also give clinicians what they need most: the ability to spend more time with patients and less time wrestling with outdated technology.
Join over 3,200 subscribers and keep up-to-date with the latest innovations & best practices in Healthcare IT.
Since the release of the Cures Act Final Rule in May 2020, the US healthcare industry has been experiencing a …
The ONC’s Cures Act, which is otherwise referred to as the 21st Century Cures Act, was enacted and signed into …
In the modern healthcare industry, data plays a very important role in terms of improving patient outcomes. …